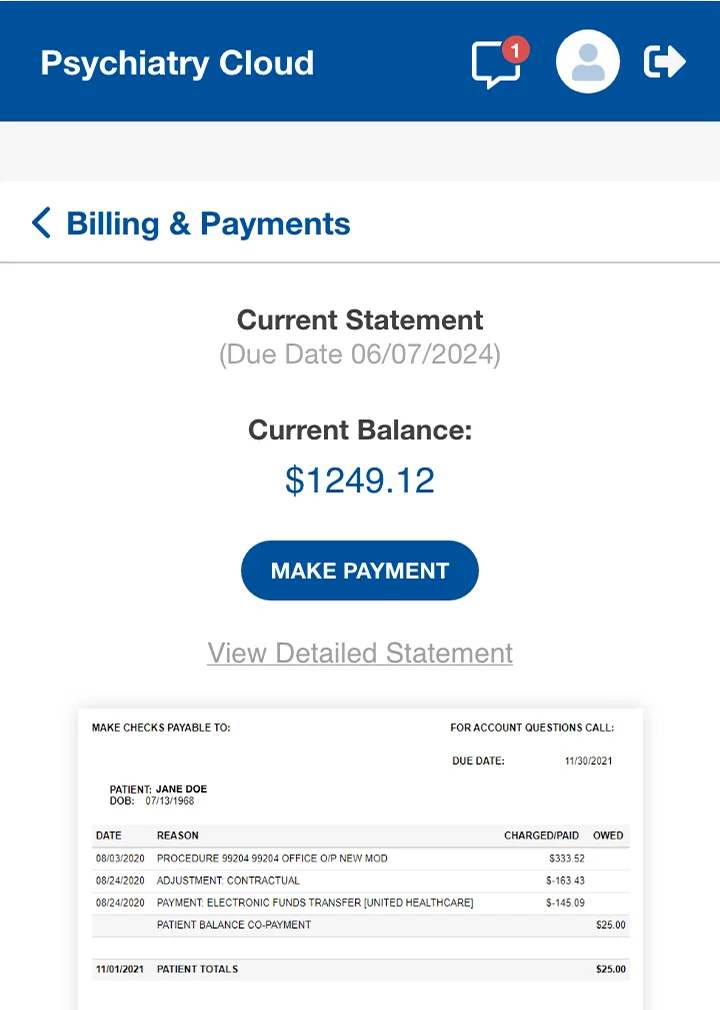
Coverage checks run automatically as soon as a patient schedules. Staff get accurate copay and deductible information before the visit—not weeks later. This prevents surprises, cuts down on denials, and reduces unpaid balances.
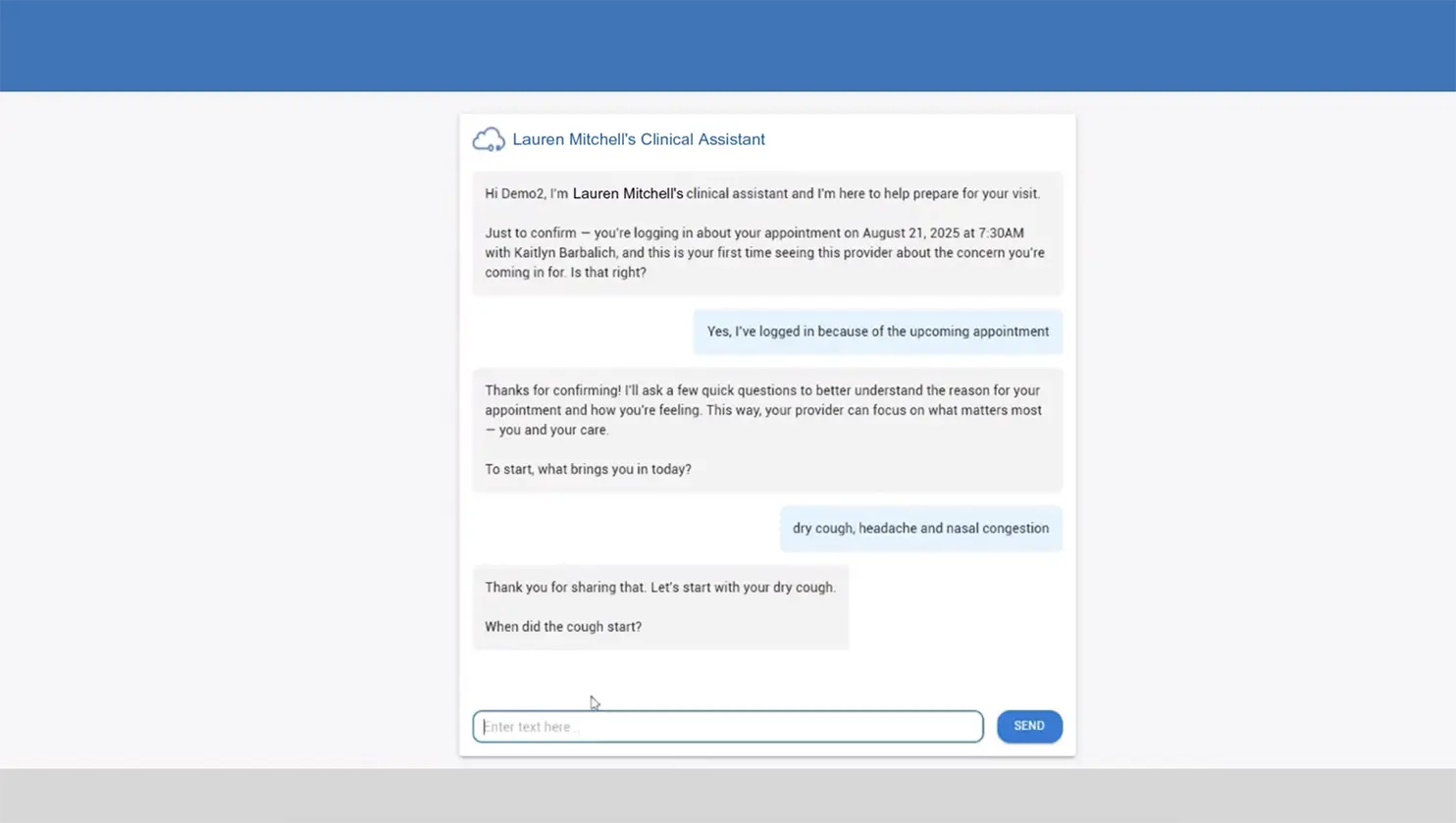
AI-powered intake captures demographics, insurance data, medication details, and required psychiatric assessments before the visit. Claims start with complete information, eliminating the need to track down missing addresses, policy numbers, or codes after the appointment.
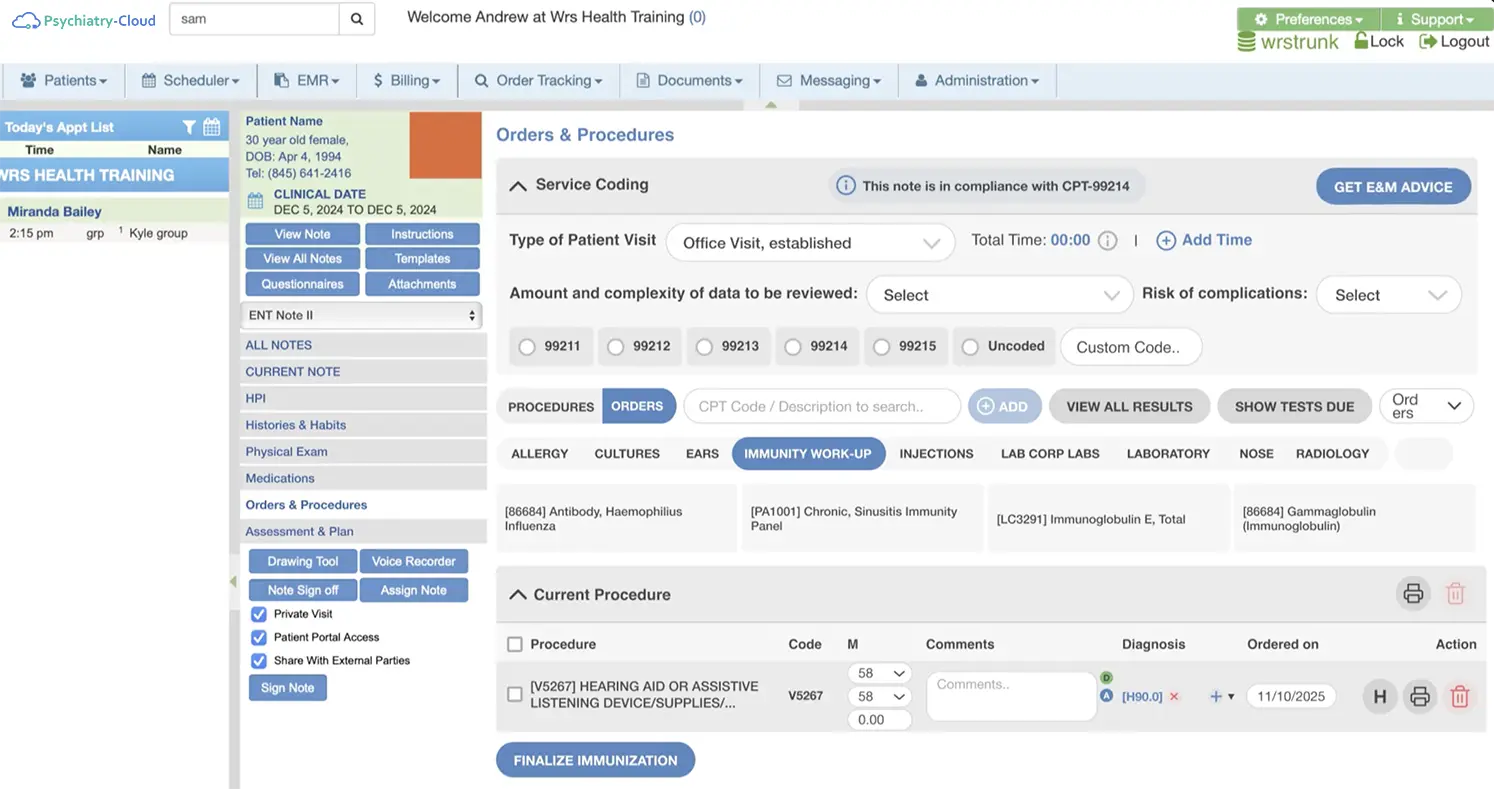
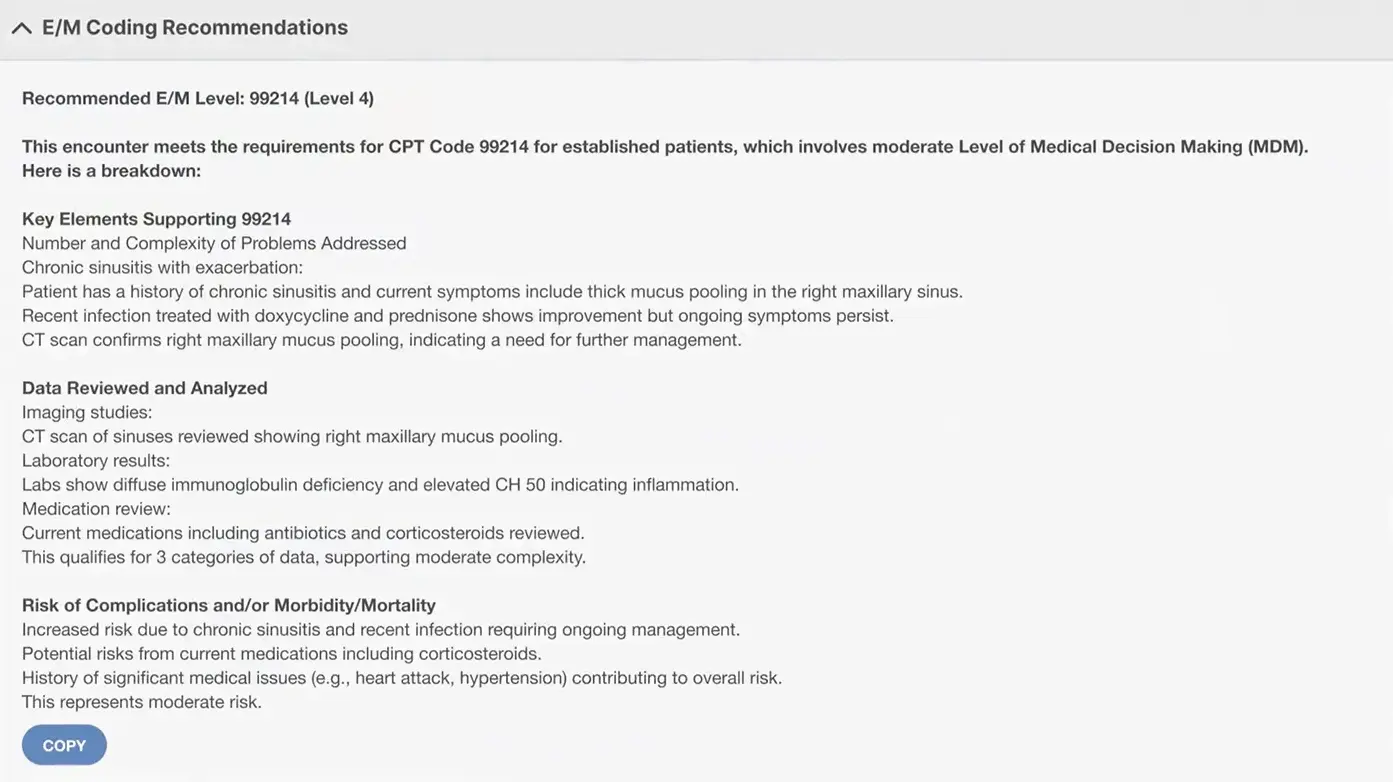
The most effective RCM support is the kind you barely notice. Automated coding, eligibility checks, and claim routing all run quietly behind the scenes. Charge capture is tied to the clinical note, and claims are created automatically once documentation is complete.
The result: fewer reworks, fewer back-and-forths, and a financial process that supports your practice instead of competing with it.
Pair our platform with full-service billing support. Our specialists manage claims, follow up on denials, and help strengthen your collections process—working alongside your team to reduce administrative strain and maximize revenue.
Fill out the form below to request a personalized demo.