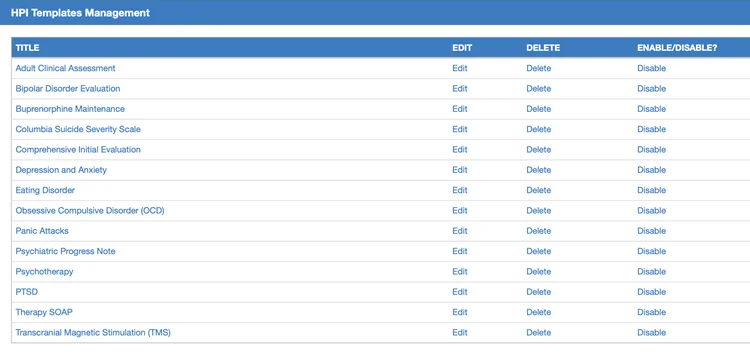
Every specialty is faced with common complaints, conditions, and diseases. Documentation can be simple with templated charting. All of our templates are created and reviewed by experts in your specialty and ready for use right out of the box. Additional customization is easy and user-specific.
Meet the diverse needs of your practice and patients with our built-in, quick charting-enabled templates. Easily create new templates with Psychiatry-Cloud EHR’s built-in customization engine, ensuring seamless integration with your workflow.
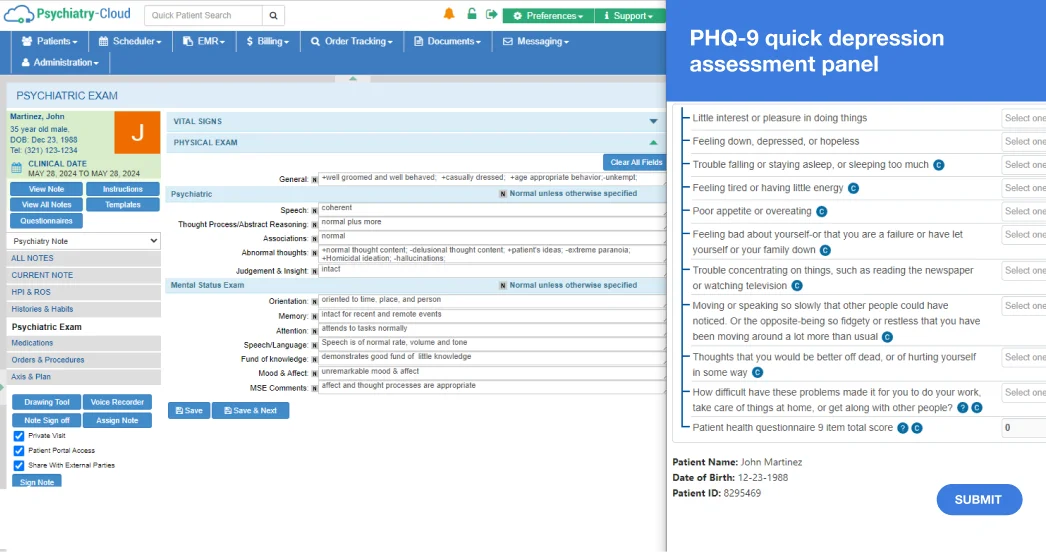
Mental status exam and ROS findings are unique to your specialty and to each provider. Start with the preset library and then use the one-click customization feature to tailor these assessments to your needs.
Optimize your patient intake and enable individuals to submit their depression severity assessments and anxiety level evaluations securely to ensure accurate and timely adjustments to their treatment plan.
Fill out the form below to request a personalized demo.