The rules are changing every year, making it almost impossible for a mental health professional to keep up with new guidelines and updated reporting requirements. Lack of compliance with MIPS standards means a missed revenue opportunity and payment penalties. Now, more than ever, physicians and their practices are under increased pressure from new regulations and growing complexities in medical services. Even with a superior mental health EHR, it still requires a significant amount of time to set up the correct process, monitor compliance, train your staff and achieve a successful Merit-based Incentive Payment System (MIPS). If you fall behind on the process, you risk jeopardizing your stimulus payments and could result in future penalties.
“Before we signed up for MIPS Management Services, we tried to attest by ourselves. We are a small practice and it turned out to be too difficult. The MIPS team is so easy to work with and they help with handling all the required QPP paperwork. This service has been a timesaver, and I am very confident in how they are managing our measures. The team goes over and beyond in helping us, especially during attestation time.”
– Reta Ramirez
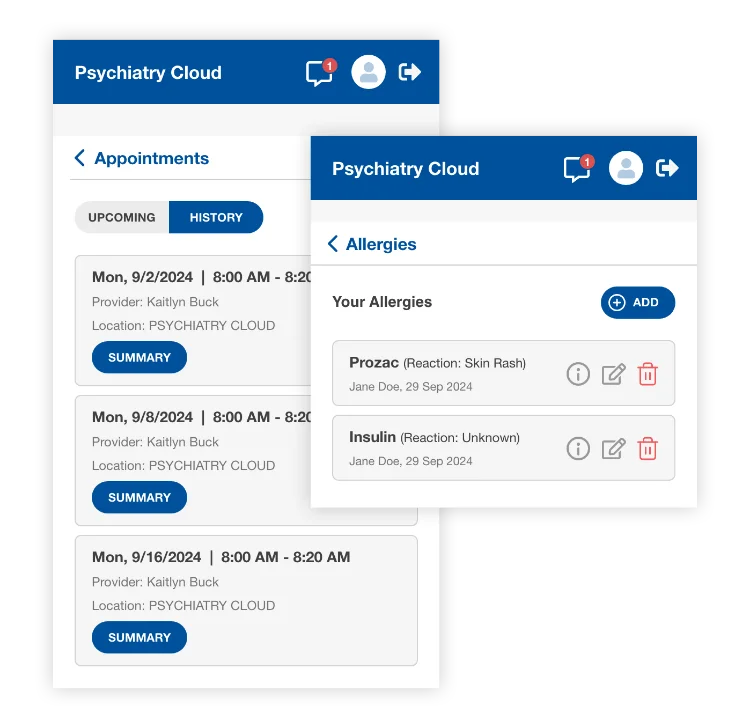
Psychiatry-Cloud complies with MIPS standards, providing patients with timely access to lab results, medication lists, allergies, and visit summaries through our secure patient portal.
First, we assign a clinically trained account manager to oversee the compliance process. Then, our MIPS compliance team monitors your practice, removing the burden from your shoulders and making sure you obtain maximum MIPS payments.

Beyond MIPS compliance, clinicians face a variety of other federal or state clinical compliance regulations. We can help with a variety of other compliance measures.
With Psychiatry-Cloud’s Clinical and MIPS Compliance Services, your practice may avoid Medicare penalties, while reducing the risk of non-compliance and potential audits. Psychiatry-Cloud’s Compliance team will manage the process, relieving you of the regulatory burdens while delivering peace of mind.
Schedule a time to talk or book a complementary practice assessment today