Designed specifically for psychiatrists and mental health professionals, the Psychiatry-Cloud EHR automates most tasks associated with order entry and medication management—allowing you to spend more time focused on your patients instead of data entry.
Powered by award-winning EHR developer, WRS Health, Psychiatry-Cloud’s platform integrates every aspect of your practice—from in-office tasks to Telehealth Appointment Scheduling, to E-prescribing through Revenue Cycle Management.
Create your own appointment types, such as new patients and support groups. Your calendar view allows you to view your daily, weekly, or monthly schedule.
The Psychiatry-Cloud EHR comes pre-loaded with psychiatric notes and templates specifically designed for psychotherapy and psychiatry, including DSM-IV-R / DSM-V criteria.
Content organization and workflow enables you to efficiently chart evaluations, therapy sessions, follow-up visits, and other encounters.
Our built-in quick charting-enabled templates will meet the immediate and diverse needs of your practice and patients. With Psychiatry-Cloud EHR’s built in customization engine, you can easily create new templates that integrate 100% with the EHR and your workflow.
Our telehealth feature is seamlessly integrated into the EHR, allowing psychiatry practices to conduct secure, high-quality virtual sessions. Providers can schedule and host both individual and group therapy sessions while accessing individual records and clinical notes in real time, while patients join securely through the patient portal from any device.
Psychiatry-Cloud EHR streamlines most tasks associated with order entry and medication management. Functions include an integrated Prescription Drug Monitoring Program (PMP) gateway to improve compliance, e-prescribing tools, easily accessible prescription histories, and more. Integrated billing.
Designed for psychiatrists, psychologists, therapists, and other mental health professionals, Psychiatry-Cloud’s billing and revenue cycle management (RCM) features integrate every part of your practice so you can get paid quickly and accurately.
Security is always a concern in any psychiatry or behavioral health practice. That’s why Psychiatry-Cloud behavioral health EHR allows you to control how staff members access specific pieces of data in the system.

Psychiatry-Cloud allows you to see patients remotely using our telehealth functionality. Fully integrated into the EHR, it allows you to manage the virtual patient encounter from appointment scheduling through revenue cycle management on one unified platform.
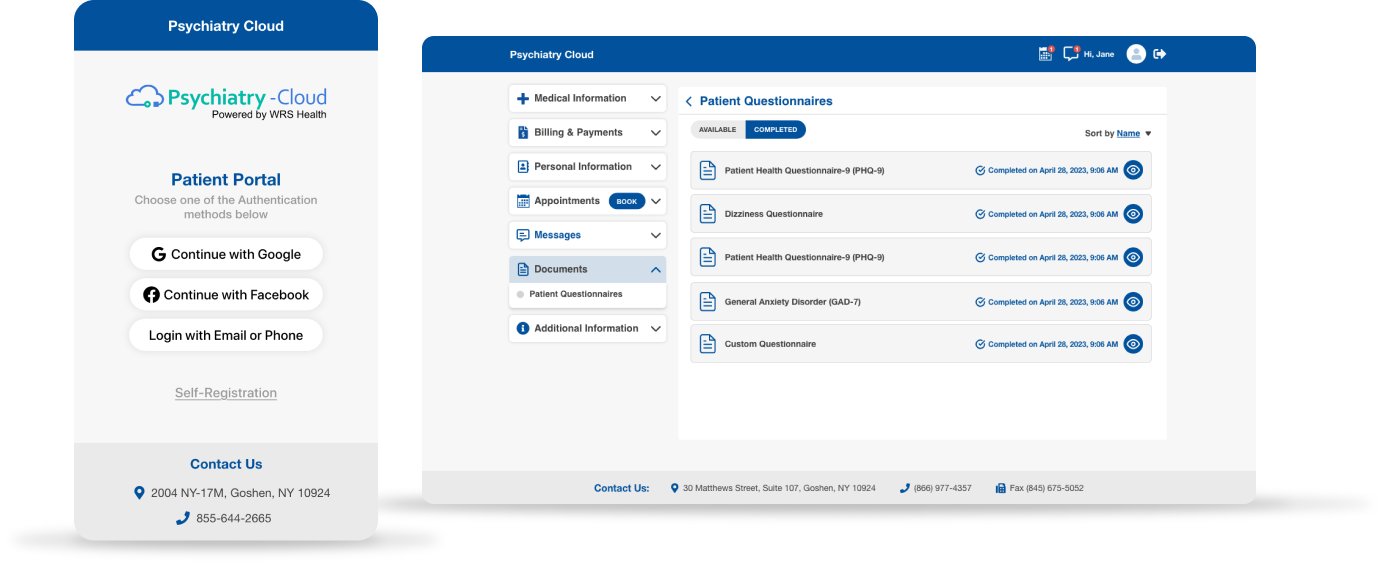
Patients are increasingly demanding access to their health information online. Our patient portal not only satisfies these demands, but also enables your patients to access educational material and even their lab results at their convenience.
Psychiatry-Cloud has been designed to work as an EHR/EMR for both solo behavioral health practitioners and larger organizations with multiple specialties and disciplines; supporting psychiatrists, psychologists, mental health counselors, therapists, as well as other medical and behavioral health organizations.
Fill out the form below to request a personalized demo.